|
'Heat Zapping' Kidney Tumors May Help Some Patients Avoid Surgery
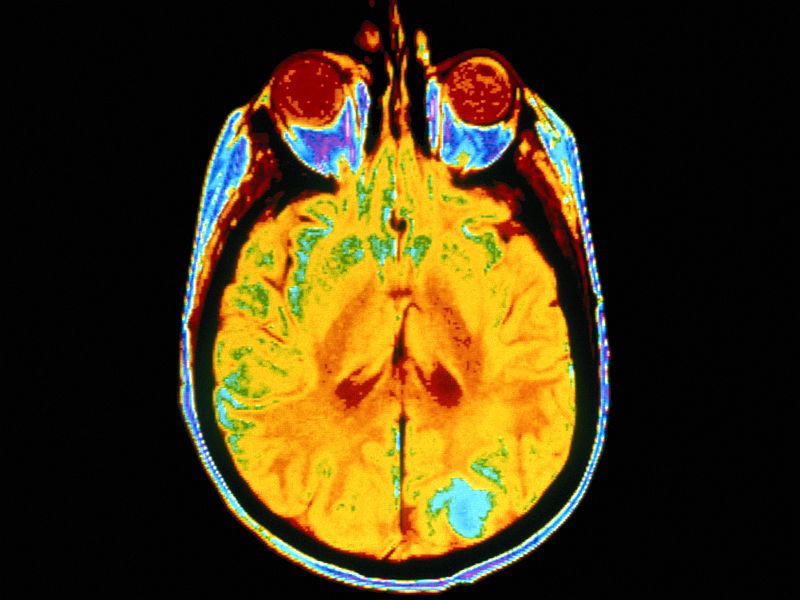
The new therapy uses a tweaked, harmless form of the polio virus to significantly boost the chances patients with recurrent glioblastomas can survive over the long term.TUESDAY, June 26, 2018 (HealthDay News) -- An ancient scourge -- the polio virus -- may be an unexpected friend to people battling one of the deadliest brain cancers, new research shows.
In the study from Duke University in Durham, N.C., 21 percent of patients who got the new treatment were still alive three years later, compared to just 4 percent of those who received standard therapy.
"There is a tremendous need for fundamentally different approaches," study senior author Dr. Darell Bigner, emeritus director of Duke's brain tumor center, said in a university news release. "With the survival rates in this early phase of the polio virus therapy, we are encouraged and eager to continue with the additional studies that are already underway or planned."
Brain cancer expert Dr. Michael Schulder noted that the "results from this trial have been eagerly awaited after preliminary information was announced on 60 Minutes several years ago."
He helps direct neurosurgery at North Shore University Hospital in Manhasset, N.Y., but wasn't involved in the new trial.
The data on outcomes from the new study remain somewhat incomplete, Schulder said, so "we will have to await the availability of the full paper to assess the effectiveness of this new treatment for patients with glioblastoma."
As the Duke team explained, the new approach uses an altered, harmless form of the polio virus to target and destroy glioblastoma cells while triggering a powerful immune response.
The initial study included 61 patients who received the genetically modified polio virus developed at the Duke Cancer Institute. Their outcomes were compared to the records of previous patients who had received standard treatment.
Median overall survival was 12.5 months in the polio virus group and 11.3 months in the control group. But the gap between treatments widened for patients who lived longer, Bigner's group noted.
Survival rates at two years were 21 percent in the polio virus group and 14 percent in the group that didn't get the therapy, and at three years they were 21 percent and 4 percent, respectively.
The findings from the phase 1 trial were published June 26 in the New England Journal of Medicine and presented on the same day at the International Conference on Brain Tumor Research and Therapy, in Norway.
The polio virus therapy was designated a "breakthrough therapy" by the U.S. Food and Drug Administration in 2016.
Neurosurgeon Dr. Jason Ellis treats brain tumors at Lenox Hill Hospital in New York City. He called the new findings "exciting," but agreed that more data are needed.
"The preliminary data reported suggest that larger randomized studies should be performed to definitively determine whether this strategy will be effective in brain tumor patients," said Ellis, who wasn't involved with the study.
Those trials may be on the way. And along with a phase 2 trial of the therapy for glioblastoma, the Duke team has started enrolling patients to test the therapy in treating brain tumors in children. Clinical trials of the therapy in breast cancer and melanoma skin cancer patients are also planned, according to the researchers.
-- Robert Preidt

Copyright © 2018 HealthDay. All rights reserved.
SOURCES: Michael Schulder, M.D., vice chair, Neurosurgery, North Shore University Hospital, Manhasset, N.Y., and Long Island Jewish Medical Center, New Hyde Park, N.Y.; Jason Ellis, M.D., neurosurgeon, Lenox Hill Hospital, New York City; Duke University, news release, June 26, 2018
Many Childhood Cancer Survivors in Denial About Future Health Risks

"Some of the increased health risks faced by survivors of childhood cancer can be minimized through early detection and intervention, as well as adoption of healthy behaviors," said study co-leader Todd Gibson, from St. Jude Children's Research Hospital in Memphis, Tenn.MONDAY, June 25, 2018 (HealthDay News) -- Many adult survivors of childhood cancer don't worry about their future health and may skip crucial screenings and lifestyle changes, a new study shows.
His team focused on questionnaire responses from more than 15,600 adult survivors of childhood cancer (median age 26) and nearly 4,000 cancer-free siblings.
About 31 percent of the survivors said they were not concerned about their future health, and 40 percent were not concerned about developing cancer. Those rates were slightly higher than or similar to their siblings.
Survivors who received high doses of radiation when they were children were more likely to be concerned about their future health. But 35 percent of these high-risk survivors were not concerned about developing cancer and 24 percent were not concerned about their future health, according to the study published June 25 in the journal Cancer.
Adults survivors of childhood cancer who aren't concerned about their future health may be less likely to get screened for cancer or to take steps to reduce their risk, the researchers suggested.
"Many survivors do not have survivor-focused medical care, so it is important for them to be aware of their health risks and advocate for appropriate guideline-based care," Gibson said in a journal news release.
"A lack of concern about potential health risks may be a barrier to this self-advocacy and adoption of healthy behaviors; however, it is important to note that not all survivors are at high risk, so for some a lack of concern is likely appropriate," Gibson added.
-- Robert Preidt

Copyright © 2018 HealthDay. All rights reserved.
CONTINUE SCROLLING FOR NEXT NEWS ARTICLE
SOURCE: Cancer, news release, June 25, 2018
More Body Fat Might Lower Odds of Breast Cancer in Younger Women
 By Alan Mozes
By Alan MozesHealthDay Reporter
THURSDAY, June 21, 2018 (HealthDay News) -- A new international review suggests that having more body fat may protect premenopausal women from developing some types of breast cancer.
"We found strong evidence of an inverse association of body mass index [BMI] with risk of breast cancer diagnosis before menopause, with lower breast cancer rates among women who were heavier compared with women who were leaner," said study author Minouk Schoemaker. She's with the Institute of Cancer Research's division of genetics and epidemiology, in London.
But experts stressed that the study couldn't prove cause and effect, and the harm from excess pounds far outweighs any benefit in curbing women's odds for developing breast cancer.
The finding stems from data drawn from 19 studies that were conducted across 15 countries. Collectively, the studies tracked more than 758,000 women for an average of nine years, during which time more than 13,000 of them developed breast cancer.
The statistics were analyzed by a consortium of 70 researchers specifically formed to investigate risk factors for breast cancer among younger women, aged 18 to 54.
At all ages between 18 and 54, having a higher BMI was associated with a notably lower risk for both estrogen receptor- and progesterone receptor-positive breast cancer. BMI levels were not linked with the risk for developing either triple-negative breast cancer or hormone receptor-negative breast cancer, the findings showed.
That said, higher BMI was most protective among women between the ages of 18 and 24. For every BMI increase of "five units," breast cancer risk fell by 23 percent. Schoemaker noted that for average-height women, a five-unit BMI increase is equivalent to roughly 22 pounds of additional weight.
Among women 25 to 34, 35 to 44 and 45 to 54, a similar increase in BMI translated into a 15, 13 and 12 percent drop in breast cancer risk, respectively, the study authors reported.
That said, Schoemaker cautioned that "this type of study can only assess associations, and it is possible that the effect of BMI we observe is due to one or more other factors that we have not measured."
Schoemaker also stressed that despite the findings, obesity continues to pose a serious health risk to women.
"Although we found a link of higher BMI and lower breast cancer risk before menopause, the great majority of breast cancers are diagnosed after the menopause, when excess weight increases risk," she said.
"Obesity is a risk factor for at least 13 types of cancer, including breast cancer after the menopause, as well as for several other diseases. There are therefore many benefits to maintaining a healthy weight," Schoemaker explained.
That thought was seconded by Dr. Gina Villani, division chief of medical oncology at Weill Cornell Medicine, in New York City.
"At the end of the day, the protective effect of obesity for young women does not outweigh the other associated risks that come with obesity, and is not and never will be a reason to 'pack on the pounds,'" Villani said.
"In addition, we know that obesity is linked to increased risk of other cancers. As the current study only looked at breast cancer risk, it is possible that the risk of breast cancer may be reduced while the risk of other cancers -- such as uterine and colon -- could be increased," she suggested.
As to what might explain the findings, Schoemaker said, "the reasons for lower breast cancer risks among heavier premenopausal women are unclear" at this point.
"Women who are heavier at young ages might have a more favorable hormone profile, a lower risk of benign breast disease and a more favorable breast composition -- lower mammographic density -- all factors which are thought to reduce risk," she said.
"The likely reason for excess weight being a risk factor for breast cancer after the menopause is that heavier women have increased levels of estrogens, a hormone that is thought to increase risk, because it is produced in fat cells," Schoemaker added.
The findings were published online June 21 in the journal JAMA Oncology.

Copyright © 2018 HealthDay. All rights reserved.
SOURCES: Minouk Schoemaker, Ph.D., co-leader, Premenopausal Breast Cancer Collaborative Group, division of genetics and epidemiology, Institute of Cancer Research, London, England; Gina Villani, M.D., MPH, division chief, medical oncology, and assistant professor, medicine, Weill Cornell Medicine, New York City; June 21, 2018, JAMA Oncology, online
When Reconstructing a Breast, Patient's Own Tissue Is Best

More than 60 percent of women who undergo breast removal to treat breast cancer decide to have breast reconstruction, and that rate is rising. But the researchers said that there has been little information about long-term satisfaction and quality of life after breast reconstruction.WEDNESDAY, June 20, 2018 (HealthDay News) -- For women who have their breast removed while fighting cancer, using their own tissue for breast reconstruction is better than implants, a new study suggests.
The study included more than 2,000 women in the United States who had breast reconstruction using either breast implants or their own skin, fat or muscle from elsewhere in the body ("autologous" reconstruction), such as the abdomen.
Two years after breast reconstruction, women who had autologous reconstruction reported greater satisfaction with their breasts and better psychosocial and sexual well-being compared with those who underwent implant reconstruction.
"Patient-centered data can best inform patients and clinicians about the potential risks and expected outcomes of breast reconstruction when making a decision between implant-based or autologous breast reconstruction," said senior study author Dr. Andrea Pusic. She is chief of plastic and reconstructive surgery at Brigham and Women's Hospital in Boston.
"Given the personal and intimate nature of breast reconstruction, patient-centered data are arguably the best measures of outcomes," Pusic said in a hospital news release. "An understanding of the expected satisfaction and quality of life is central to the decision-making process."
The study was published June 20 in the journal JAMA Surgery.
-- Robert Preidt

Copyright © 2018 HealthDay. All rights reserved.
SOURCE: Brigham and Women's Hospital, news release, June 20, 2018
'Heat Zapping' Kidney Tumors May Help Some Patients Avoid Surgery
 By E.J. Mundell
By E.J. MundellHealthDay Reporter
TUESDAY, June 26, 2018 (HealthDay News) -- When kidney cancer strikes, surgical removal of the organ is often the standard course of action.
But new research supports a nonsurgical approach for some patients: using a needle to "zap" kidney tumors away with either heat or cold.
The procedure -- known as percutaneous ablation -- isn't applicable to all kidney cancer patients. But for a "well-selected" group with small tumors (under 4 centimeters in diameter), it may result in long-term survival equal to that of surgery, with five times fewer complications, the study found.
That means "fewer complications and less chronic renal [kidney] insufficiency" for patients who get the procedure, said a team led by Dr. Adam Talenfeld, of Weill Cornell Medicine in New York City.
The researchers published the findings June 25 in the Annals of Internal Medicine.
One kidney cancer specialist not involved with the study said treatment options keep evolving.
"Treatment of kidney cancer has seen revolutionary changes -- from the days of open incision to laparoscopic and robotic removal -- allowing for improved recovery and preservation of kidney function," explained Dr. Louis Kavoussi. He directs urology at Northwell Health in New Hyde Park, N.Y.
But he said when it comes to the successful use of ablation, "tumors need to be less than 3 centimeters in size [slightly above an inch] and in a place that is not next to another organ, as the energy to destroy the tumor can cause injury to other sites."
In the new study, Talenfeld's group tracked post-procedure complications and five-year outcomes for more than 4,300 patients diagnosed with early stage kidney cancer, with tumors under 4 centimeters wide. Patients averaged 66 years of age.
The investigators found that patients had similar overall five-year kidney cancer survival whether they received surgery to remove a part of the kidney (98 percent survival) or ablation (95 percent). The odds of surviving kidney cancer after five years were similarly high as well when comparing ablation to complete kidney removal.
When the researchers looked at deaths from any cause, five-year survival was somewhat higher for patients who got surgery (86 percent) versus those who underwent ablation (77 percent).
However, there may have been a payoff for ablation in terms of quality of life -- people who got the procedure were more likely to retain good kidney function than those who got surgery, the research team noted.
Also, the rate of complications during the month after their treatment was much higher for patients who underwent surgery (about 30 percent) versus those who got ablation (6 percent).
Talenfeld's group stressed that the superiority of ablation may apply only to patients with smaller tumors, and might not apply to younger patients.
"This somewhat limits who may be a candidate," Kavoussi said. And he stressed that "in order for ablation to be done properly, there needs to be an experienced and collaborative team of urologists and radiologists working together."
Dr. Maria DeVita is training program director in nephrology at Lenox Hill Hospital in New York City. She said that before the new study, there had been "little data on the safety and outcomes of ablation" for kidney cancer.
So, "this is a much-needed report giving doctors reassurance that patients undergoing ablation are not in harm's way," said DeVita, who wasn't involved with the research. She added that especially for elderly patients, anything that can be done to preserve even partial kidney function can help stave off potentially fatal kidney failure.

Copyright © 2018 HealthDay. All rights reserved.
SOURCES: Louis Kavoussi, M.D., chairman, urology, Northwell Health, New Hyde Park, N.Y.; Maria DeVita, M.D., training program director, nephrology, Lenox Hill Hospital, New York City; June 25, 2018, Annals of Internal Medicine

মন্তব্যসমূহ
একটি মন্তব্য পোস্ট করুন