Facts About Diabetic Eye
Disease ( COURTECY;- webMD ) & 0THTER ARTICLES FROM INTERNATE (
Points
to Remember
1. Diabetic
eye disease comprises a group of eye conditions that affect people with
diabetes. These conditions include diabetic retinopathy, diabetic macular edema
(DME), cataract, and glaucoma.
2. All
forms of diabetic eye disease have the potential to cause severe vision loss
and blindness.
3. Diabetic
retinopathy involves changes to retinal blood vessels that can cause them to
bleed or leak fluid, distorting vision.
4. Diabetic
retinopathy is the most common cause of vision loss among people with diabetes
and a leading cause of blindness among working-age adults.
5. DME is
a consequence of diabetic retinopathy that causes swelling in the area of the
retina called the macula.
6. Controlling
diabetes—by taking medications as prescribed, staying physically active, and
maintaining a healthy diet—can prevent or delay vision loss.
7. Because
diabetic retinopathy often goes unnoticed until vision loss occurs, people with
diabetes should get a comprehensive dilated eye exam at least once a year.
8. Early
detection, timely treatment, and appropriate follow-up care of diabetic eye
disease can protect against vision loss.
9. Diabetic
retinopathy can be treated with several therapies, used alone or
in combination.
10.
NEI supports research to develop new therapies for diabetic
retinopathy, and to compare the effectiveness of existing therapies for
different patient groups.
What is
diabetic eye disease?

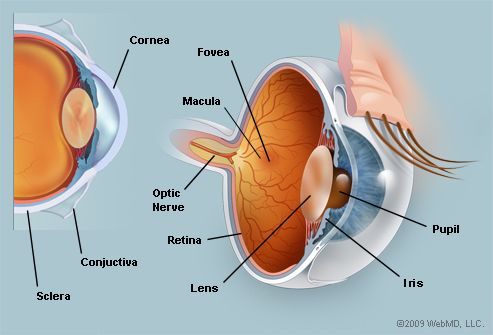
Diabetic eye disease can affect many parts of the eye, including the retina, macula, lens and the optic nerve.
Diabetic eye disease is a group of eye conditions that can
affect people with diabetes.
- Diabetic
retinopathy affects
blood vessels in the light-sensitive tissue called the retina that lines
the back of the eye. It is the most common cause of vision loss among
people with diabetes and the leading cause of vision impairment and
blindness among working-age adults.
- Diabetic
macular edema (DME). A consequence of diabetic
retinopathy, DME is swelling in an area of the retina called
the macula.
Diabetic eye disease also includes cataract and glaucoma:
- Cataract is a
clouding of the eye’s lens. Adults with diabetes are 2-5 times more likely
than those without diabetes to develop cataract. Cataract also tends to
develop at an earlier age in people with diabetes.
- Glaucoma is a group
of diseases that damage the eye’s optic nerve—the bundle of nerve fibers
that connects the eye to the brain. Some types of glaucoma are associated
with elevated pressure inside the eye. In adults, diabetes nearly doubles
the risk of glaucoma.
All forms of diabetic eye disease have the potential to cause
severe vision loss and blindness.
Diabetic Retinopathy
What
causes diabetic retinopathy?
Chronically high blood sugar from diabetes is associated with
damage to the tiny blood vessels in the retina, leading to diabetic
retinopathy. The retina detects light and converts it to signals sent through the
optic nerve to the brain. Diabetic retinopathy can cause blood vessels in the
retina to leak fluid or hemorrhage (bleed), distorting vision. In its most
advanced stage, new abnormal blood vessels proliferate (increase in number) on
the surface of the retina, which can lead to scarring and cell loss in the
retina.
Diabetic retinopathy may progress through four stages:
1. Mild
nonproliferative retinopathy. Small areas of
balloon-like swelling in the retina’s tiny blood vessels, called
microaneurysms, occur at this earliest stage of the disease. These
microaneurysms may leak fluid into the retina.
2. Moderate
nonproliferative retinopathy. As the disease
progresses, blood vessels that nourish the retina may swell and distort. They
may also lose their ability to transport blood. Both conditions cause
characteristic changes to the appearance of the retina and may contribute
to DME.
3. Severe
nonproliferative retinopathy. Many more blood
vessels are blocked, depriving blood supply to areas of the retina. These areas
secrete growth factors that signal the retina to grow new blood vessels.
4. Proliferative
diabetic retinopathy (PDR). At this advanced stage, growth factors
secreted by the retina trigger the proliferation of new blood vessels, which
grow along the inside surface of the retina and into the vitreous gel, the
fluid that fills the eye. The new blood vessels are fragile, which makes them
more likely to leak and bleed. Accompanying scar tissue can contract and cause
retinal detachment—the pulling away of the retina from underlying tissue, like
wallpaper peeling away from a wall. Retinal detachment can lead to permanent
vision loss.
What is
diabetic macular edema (DME)?
DME is the build-up of fluid (edema) in a region of the retina
called the macula. The macula is important for the sharp, straight-ahead vision
that is used for reading, recognizing faces, and driving. DME is the most
common cause of vision loss among people with diabetic retinopathy. About half
of all people with diabetic retinopathy will develop DME. Although it is more
likely to occur as diabetic retinopathy worsens, DME can happen at any stage of
the disease.
Who is
at risk for diabetic retinopathy?
People with all types of diabetes (type 1, type 2, and
gestational) are at risk for diabetic retinopathy. Risk increases the longer a
person has diabetes. Between 40 and 45 percent of Americans diagnosed with
diabetes have some stage of diabetic retinopathy, although only about half are
aware of it. Women who develop or have diabetes during pregnancy may have rapid
onset or worsening of diabetic retinopathy.
Symptoms
and Detection
What
are the symptoms of diabetic retinopathy and DME?
The same scene as viewed by a person normal vision (Top) and with (Center) advanced diabetic retinopathy. The floating spots are hemorrhages that require prompt treatment. DME (Bottom) causes blurred vision.
The early stages of diabetic retinopathy usually have no
symptoms. The disease often progresses unnoticed until it affects vision.
Bleeding from abnormal retinal blood vessels can cause the appearance of
“floating” spots. These spots sometimes clear on their own. But without prompt
treatment, bleeding often recurs, increasing the risk of permanent vision loss.
If DME occurs, it can cause blurred vision.
How are
diabetic retinopathy and DME detected?
Diabetic retinopathy and DME are detected during a comprehensive
dilated eye exam that includes:
1. Visual
acuity testing. This eye chart test measures a person’s ability to see at
various distances.
2. Tonometry. This
test measures pressure inside the eye.
3. Pupil dilation. Drops
placed on the eye’s surface dilate (widen) the pupil, allowing a physician to
examine the retina and optic nerve.
4. Optical
coherence tomography (OCT). This technique is similar to ultrasound
but uses light waves instead of sound waves to capture images of tissues inside
the body. OCT provides detailed images of tissues that can be penetrated by
light, such as the eye.
A comprehensive dilated eye exam allows the doctor to check the
retina for:
1. Changes
to blood vessels
2. Leaking
blood vessels or warning signs of leaky blood vessels, such as
fatty deposits
3. Swelling
of the macula (DME)
4. Changes
in the lens
5. Damage
to nerve tissue
If DME or severe diabetic retinopathy is suspected, a fluorescein
angiogram may be used to look for damaged or leaky blood vessels. In
this test, a fluorescent dye is injected into the bloodstream, often into an
arm vein. Pictures of the retinal blood vessels are taken as the dye reaches
the eye.
Prevention
and Treatment
How can
people with diabetes protect their vision?
Vision lost to diabetic retinopathy is sometimes irreversible.
However, early detection and treatment can reduce the risk of blindness by 95
percent. Because diabetic retinopathy often lacks early symptoms, people with
diabetes should get a comprehensive dilated eye exam at least once a year.
People with diabetic retinopathy may need eye exams more frequently. Women with
diabetes who become pregnant should have a comprehensive dilated eye exam as
soon as possible. Additional exams during pregnancy may be needed.
Studies such as the Diabetes Control and Complications Trial
(DCCT) have shown that controlling diabetes slows the onset and worsening of
diabetic retinopathy. DCCT study participants who kept their blood glucose
level as close to normal as possible were significantly less likely than those
without optimal glucose control to develop diabetic retinopathy, as well as
kidney and nerve diseases. Other trials have shown that controlling elevated
blood pressure and cholesterol can reduce the risk of vision loss among people
with diabetes.
Treatment for diabetic retinopathy is often delayed until it
starts to progress to PDR, or when DME occurs. Comprehensive dilated eye exams
are needed more frequently as diabetic retinopathy becomes more severe. People
with severe nonproliferative diabetic retinopathy have a high risk of
developing PDR and may need a comprehensive dilated eye exam as often as every
2 to 4 months.
How is
DME treated?
DME can be treated with several therapies that may be used alone
or in combination.
Anti-VEGF Injection Therapy. Anti-VEGF drugs are
injected into the vitreous gel to block a protein called vascular endothelial
growth factor (VEGF), which can stimulate abnormal blood vessels to grow and
leak fluid. Blocking VEGF can reverse abnormal blood vessel growth and decrease
fluid in the retina. Available anti-VEGF drugs include Avastin (bevacizumab),
Lucentis (ranibizumab), and Eylea (aflibercept). Lucentis and Eylea are
approved by the U.S. Food and Drug Administration (FDA) for treating DME.
Avastin was approved by the FDA to treat cancer, but is commonly used to treat
eye conditions, including DME.
The NEI-sponsored Diabetic Retinopathy Clinical Research Network
compared Avastin, Lucentis, and Eylea in a clinical trial. The study found all
three drugs to be safe and effective for treating most people with DME.
Patients who started the trial with 20/40 or better vision experienced similar
improvements in vision no matter which of the three drugs they were given.
However, patients who started the trial with 20/50 or worse vision had greater
improvements in vision with Eylea.
Most people require monthly anti-VEGF injections for the first
six months of treatment. Thereafter, injections are needed less often:
typically three to four during the second six months of treatment, about four
during the second year of treatment, two in the third year, one in the fourth
year, and none in the fifth year. Dilated eye exams may be needed less often as
the disease stabilizes.
Avastin, Lucentis, and Eylea vary in cost and in how often they
need to be injected, so patients may wish to discuss these issues with an eye
care professional.


The retina of a person with diabetic retinopathy and DME, as viewed by optical coherence tomography (OCT). The two images were taken before (Top) and after anti-VEGF treatment (Bottom). The dip in the retina is the fovea, a region of the macula where vision is normally at its sharpest. Note the swelling of the macula and elevation of the fovea before treatment.
Focal/grid macular laser surgery. In
focal/grid macular laser surgery, a few to hundreds of small laser burns are
made to leaking blood vessels in areas of edema near the center of the macula.
Laser burns for DME slow the leakage of fluid, reducing swelling in the retina.
The procedure is usually completed in one session, but some people may need
more than one treatment. Focal/grid laser is sometimes applied before anti-VEGF
injections, sometimes on the same day or a few days after an anti-VEGF
injection, and sometimes only when DME fails to improve adequately after six
months of anti-VEGF therapy.
Corticosteroids. Corticosteroids,
either injected or implanted into the eye, may be used alone or in combination
with other drugs or laser surgery to treat DME. The Ozurdex (dexamethasone)
implant is for short-term use, while the Iluvien (fluocinolone acetonide)
implant is longer lasting. Both are biodegradable and release a sustained dose
of corticosteroids to suppress DME. Corticosteroid use in the eye increases the
risk of cataract and glaucoma. DME patients who use corticosteroids should be
monitored for increased pressure in the eye and glaucoma.
How is
proliferative diabetic retinopathy (PDR) treated?
For decades, PDR has been treated with scatter laser surgery,
sometimes called panretinal laser surgery or panretinal photocoagulation.
Treatment involves making 1,000 to 2,000 tiny laser burns in areas of the
retina away from the macula. These laser burns are intended to cause abnormal
blood vessels to shrink. Although treatment can be completed in one session,
two or more sessions are sometimes required. While it can preserve central
vision, scatter laser surgery may cause some loss of side (peripheral), color,
and night vision. Scatter laser surgery works best before new, fragile blood
vessels have started to bleed. Recent studies have shown that anti-VEGF
treatment not only is effective for treating DME, but is also effective for
slowing progression of diabetic retinopathy, including PDR, so anti-VEGF is
increasingly used as a first-line treatment for PDR.
What is
a vitrectomy?
A vitrectomy is the surgical removal of the vitreous gel in the
center of the eye. The procedure is used to treat severe bleeding into the
vitreous, and is performed under local or general anesthesia. Ports (temporary
water-tight openings) are placed in the eye to allow the surgeon to insert and
remove instruments, such as a tiny light or a small vacuum called a vitrector.
A clear salt solution is gently pumped into the eye through one of the ports to
maintain eye pressure during surgery and to replace the removed vitreous. The
same instruments used during vitrectomy also may be used to remove scar tissue
or to repair a detached retina.
Vitrectomy may be performed as an outpatient procedure or as an
inpatient procedure, usually requiring a single overnight stay in the hospital.
After treatment, the eye may be covered with a patch for days to weeks and may
be red and sore. Drops may be applied to the eye to reduce inflammation and the
risk of infection. If both eyes require vitrectomy, the second eye usually will
be treated after the first eye has recovered.
What if
treatment doesn’t improve vision?
An eye care professional can help locate and make referrals
to low vision and
rehabilitation services and suggest devices that may help make the most of
remaining vision. Many community organizations and agencies offer information
about low vision counseling, training, and other special services for people
with visual impairment. A nearby school of medicine or optometry also may
provide low vision and rehabilitation services.
Current Research
What is
the NEI doing to advance research on diabetic eye disease?
The NEI is conducting and supporting research that seeks better
ways to detect, treat, and prevent vision loss in people with diabetes. This
research is being conducted in labs and clinical centers across the country.
For example, the Diabetic Retinopathy Clinical Research Network
(DRCR.net) conducts large multi-center trials to test new therapies for
diabetic eye disease, and to compare different therapies. The network formed in
2002 and comprises more than 350 physicians practicing at more than 140
clinical sites across the country. Many of the sites are private practice eye
clinics, enabling the network to quickly bring innovative treatments from
research into community practice.
NEI-funded scientists are also seeking ways to detect diabetic
retinopathy at earlier stages. For example, researchers are harnessing a
technology called adaptive optics (AO) to improve imaging techniques such as
OCT. AO was developed by astronomers seeking to improve the resolution of their
telescopes by filtering out distortions in the atmosphere. In the clinic,
diagnostic devices that use AO may improve the detection of subtle changes in
retinal tissue and blood vessels.
Last Reviewed:
September 2015
The National Eye Institute (NEI) is part of the National Institutes
of Health (NIH) and is the Federal government’s lead agency for vision research
that leads to sight-saving treatments and plays a key role in reducing visual
impairment and blindness.
Can Diabetes Affect Your Eyes?
IN THIS ARTICLE
Yes. You should plan to make regular eye doctor visits when you have diabetes.
High blood sugar can lead to problems like
blurry vision, cataracts, glaucoma,
and retinopathy. In fact, diabetes is
the primary cause of blindness in adults ages 20 to 74.
Blurry Vision
Don't buy new glasses as soon as you
notice that things look blurry. It could just be a small problem caused by
high blood sugar. Your lens could swell, which changes
your ability to see.
To correct it, you need to get your blood sugar back into the target range (70-130
milligrams per deciliter, or mg/dL, before meals, and less than 180 mg/dL 1 to
2 hours after a meal). It may take as long as 3 months for your vision to fully get back to normal.
Do tell your eye doctor. She can let you know if this is a
symptom of a more serious problem.
Cataracts
The lens allows your eye to see and focus on an image, just like a
camera. Cataracts cloud your normally clear lens with
debris. Anyone can get them, but people with diabetes tend to get them earlier, and they get
worse faster.
When part of your lens is cloudy,
your eye can’t focus like it should. You won't see as
well. Symptoms include blurred vision and glare.
CONTINUE READING BELOW
YOU MIGHT LIKE
WEBMD
Slideshow:
Essential Tips to Manage Your Diabetes
Diabetes
means you have to watch your diet and medicines closely. Use these WebMD tips
to manage your condition every day.
WEBMD
Quiz:
Do You Know How to Stay Dry?
Lots
of things can make you sweat -- do you know how to keep your cool? Take this
quiz and find out.
You’ll need surgery to remove a cataract.
The doctor replaces the cloudy lens with an artificial one.
Glaucoma

Pressure builds up inside your eye when
fluid can’t drain like it should. This can damage nerves and bloodvessels, and cause changes in vision.
Medications can
treat open-angle glaucoma, the most common form. They lower eye
pressure, speed up drainage, and reduce the amount of liquid your eye makes.
(Your doctor will call this aqueous humor.)
This type of glaucoma may not cause any symptoms until it’s
further along and you have major vision loss. Your doctor can catch it earlier, during
an annual exam.
With less common forms of the disease, you
might notice:
- Headaches
- Eye aches or pain
- Blurred vision
- Watery eyes
- Halos around lights
- Vision loss
Treatment can include medicine and special
eye drops. Surgery and laser treatments can help with drainage.
If you have diabetes, you’re also more
likely to get a rare condition called neovascular glaucoma. This makes
new blood vessels grow on the iris, the colored part
of your eye. They block the normal flow of fluid and raise eye pressure.
It's difficult to treat. Your doctor might
try laser surgery to cut back on the vessels. Or he could use implants to help
drain the fluid.
Diabetic Retinopathy
The retina is a group of cells on the back
of your eye that take in light. They turn it into images that the optic nerve
sends to your brain.

Damage to small blood vessels in your retina causes diabetic retinopathy. It's related to high blood sugar levels. If you don’t find and treat it
early, you could go blind. The longer you have diabetes, the more likely you
are to get it. If you keep your blood sugar under control, you lower your
chances.
People with type 1 diabetes rarely develop the condition
before puberty. In adults, it's rare to see unless you've
had type 1 diabetesfor at least 5 years. If you keep
tight control of your blood sugar with either an insulin
pump or multiple daily insulin injections, you’re far less likely to
get this condition.
If you have type 2 diabetes, you may have signs of eye problemswhen you’re diagnosed. Control your blood
sugar, blood pressure, and cholesterol to slow or prevent the disease. If
you smoke, try to quit. It’ll improve your eyes and your overall health.
There are other types of this condition:
Background retinopathy. Your blood vessels are damaged, but you can still see
OK. It can get worse if you don't manage your diabetes well.
Maculopathy. This is damage to the macula, a critical area of
your retina. It can greatly affect your vision.
Proliferative retinopathy. It happens when cells at the back of your eye
don’t get enough oxygen and new blood vessels start to grow. They’re fragile,
so they can bleed and lead to a clot. This can cause scars and pull your retina
away from the back of your eye. If it gets detached, you could have vision loss that can't be fixed. Sometimes this
condition can be treated. Surgery is an option, so is a laser procedure that
burns away the blood vessels. It can prevent blindness in up to half the people
with early retinopathy.
The Need for Eye Exams
A full yearly checkup can help find
problems early, when they're easier to treat. That could save your vision.
If you might get pregnant in the near future, get an eye exam to
avoid possible problems. Keep them up while you’re pregnant,
too.
When to Call the Doctor
These symptoms can signal an emergency:
- Black spots in your vision
- Flashes of light
- "Holes" in your vision
- Blurred vision
WebMD
Medical Reference Reviewed by Michael
Dansinger, MD on February 26,
2017
EYE DAMAGE (DIABETIC RETINOPATHY)
SHARE PRINT
o Anxiety
·
RECIPES
Diabetes can cause
"diabetic retinopathy", the most common eye disease affecting 500,000
Canadians. Diabetic retinopathy can lead to vision changes or blindness. With
good blood sugar control, regular eye exams and early treatment, the risk of eye
damage can be reduced.
We are pleased to announce that Diabetes Canada and the Canadian
Ophthalmological Society have partnered to help educate people with
diabetes about retinopathy.
How can diabetes affect my eyes?
Having too much glucose (sugar) in your blood can damage the
blood vessels in the retina, leading to diabetic retinopathy. The retina is the
tissue lining the back of the eye and works like a film in a camera that helps
you see. Changes to your eye with diabetic retinopathy can reduce your vision.
Why should I get an eye exam?
Diabetic retinopathy develops over time and often goes unnoticed
until vision loss occurs. All people with diabetes (both type 1 and type 2) are
at risk for diabetic retinopathy. Regular eye exams are very important to
detect changes early, even before you see any difference in your vision.
How often is an eye exam recommended?
If your vision changes, you should go see your eye doctor
immediately. Symptoms can include:
·
Blurred vision
·
Flashes of light in the field of vision
·
Sudden loss of vision
·
Blotches or spots in vision
If your vision is doing well, you should get an eye exam once a
year, unless otherwise directed by your ophthalmologist or
optometrist. The possibility of eye complications can be greatly reduced
with routine examinations. Many problems can be treated with greater success
when caught early.
Remember, you may not be aware of changes to your vision.
Diabetic retinopathy can worsen in pregnancy, so it is important to get a
diabetic eye exam before getting pregnant and while pregnant.
About the eye exam
During the eye exam, an ophthalmologist or optometrist puts
drops into your eyes to dilate (enlarge) your pupils. Once your eyes are
dilated, your eye-care provider examines your eyes using a special magnifying
lens that provides a clear view of the back of your eye. Dilated eye exams are
a safe and effective part of your diabetes management.
Contact your eye-care professional directly for an appointment
or have your health-care provider refer you for an eye exam. A diabetic eye
exam may be covered by your provincial health plan and be available at no cost
to you. You can confirm this with your diabetes care provider or when making an
appointment.
If you happen to have diabetic retinopathy, very effective
treatments are available. Your eye-care specialist will explain these to you.
How can I reduce my risk of diabetic retinopathy?
To prevent disease progression, people with diabetes should
manage their levels of blood sugar, blood pressure and blood cholesterol.
Research has shown that keeping blood sugar levels within target leads to fewer
eye problems. People with diabetes should follow the ABCDEs to reduce the risk
of eye damage.
A – A1C – Most people should aim for an A1C
of seven per cent* or less by managing blood sugars well. A1C is a blood test
that is a measure of your average blood sugar level over the past 120 days.
B – Blood pressure – Control your blood
pressure to less than 130/80* mmHg.
C – Cholesterol – The LDL (bad)
cholesterol target is less than 2.0* mmol/L.
D – Drugs to protect your heart –
Speak with your health-care team about medications.
E – Exercise & Eating – Regular physical
activity, healthy eating, and maintain a healthy body weight.
S – Screening for complications –
Ask your health-care team about tests for your heart, feet, kidneys, and eyes.
S – Smoking cessation – Stop smoking and
and seek support for help with quitting.
S – Self management, stress, and other barriers –
Set goals for yourself to reach the targets and live well with diabetes, such
as managing stress effectively.
* Discuss your target values with your health-care team. Note
that A1C targets for pregnant women, older adults and children 12 years of age
and under are different
For more information about diabetic retinopathy, visit the Canadian National Institute
for the Blind (CNIB).
To find a CAO optometrist in your area, visit the Canadian
Association of Optometrists.
RELATED CONTENT
Eye Problems and Diabetes
Eye problems and diabetes introduction
If you have diabetes, regular visits to your ophthalmologist for
eye exams are important to avoid eye
problems. High blood sugar (glucose)
increases the risk of diabetes eye
problems. In fact, diabetes is
the leading cause of blindness in adults age 20 to 74.
If you have eye problems and diabetes, don't buy a new pair of
glasses as soon as you notice you have blurred vision. It could just be a temporary eye
problem that develops rapidly with diabetes and is caused by high blood
sugar levels.
High blood sugar in
diabetes causes the lens of
the eye to swell, which changes your ability to see. To correct this kind of
eye problem, you need to get your blood sugar back
into the target range (90-130 milligrams per deciliter or mg/dL before meals,
and less than 180 mg/dL one to two hours after a meal). It may take as long as
three months after your blood sugar is well controlled for your vision to fully
get back to normal.
Blurred vision can also be a symptom of more serious eye problem
with diabetes. The three major eye problems that people with diabetes may
develop and should be aware of are cataracts, glaucoma,
and retinopathy.
Cataracts
and Diabetes
A cataract is
a clouding or fogging of the normally clear lens of the eye. The lens is what
allows us to see and focus on an image just like a camera. Although anyone can
get cataracts,
people with diabetes get these eye problems at an earlier age than most and the
condition progresses more rapidly than in people without diabetes.
If you have a cataract, there is a cloudy area in the lens of
your eye that results in the inability to focus light, and your vision is
impaired. Symptoms of this eye problem in diabetes include blurred or glared
vision.
During cataract surgery, the cloudy lens is removed or
cleaned out and replaced by a clear man-made lens.

Picture of Cataract of the Eye
Quick
GuideDiabetes Tips: Managing and Living With
Diabetes

Diabetic
Retinopathy Symptoms
Does diabetic retinopathy have any symptoms?
Often there are no symptoms in the early stages of the disease,
nor is there any pain. Don't wait for symptoms. Be sure to have a comprehensive
dilated eye exam at least once a year.
Blurred vision may occur when the macula - the part of the
retina that provides sharp central vision - swells from leaking fluid. This
condition is called macular edema.
If new blood vessels grow on the surface of the retina, they can
bleed into the eye and block vision.
What are the symptoms of proliferative retinopathy if bleeding
occurs?
At first, you will see a few specks of blood, or spots,
"floating" in your vision. If spots occur, see your eye care
professional as soon as possible. You may need treatment before more serious
bleeding occurs. Hemorrhages tend to happen more than once, often during sleep.
Sometimes, without treatment, the spots clear, and you will see
better. However, bleeding can reoccur and cause severely blurred vision. You
need to be examined by your eye care professional at the first sign of blurred
vision, before more bleeding occurs.
If left untreated, proliferative retinopathy can cause severe
vision loss and even blindness. Also, the earlier you receive treatment, the
more likely treatment will be effective.
SOURCE:
National Eye Institute. Facts About Diabetic Retinopathy.
National Eye Institute. Facts About Diabetic Retinopathy.
Glaucoma and
Diabetes
·
When fluid inside the eye does not drain properly from a
buildup of pressure inside the eye, it results in another eye problem with
diabetes called glaucoma.
The pressure damages nerves and the vessels in the eye, causing changes in
vision.
Treatment of open-angle
glaucoma -- the most common form of glaucoma -- requires
lowering the eye's pressure by increasing the drainage of aqueous humor or
decreasing the production of the fluid. Medications can accomplish both of
these goals.
With open-angle glaucoma, there may be no symptoms of this eye
problem at all until the disease is very advanced and there is
significant vision loss. In the less common form of this eye
problem, symptoms can include headaches,
eye aches or pain,
blurred vision, watering eyes, halos around lights, and loss of vision.
Treatment of this eye problem in diabetes can include special
eye drops, laser procedures, medicine, or surgery. Surgery and laser treatments
are directed at improving the eye's aqueous drainage. You can prevent serious
eye problems in diabetes problems by getting an annual glaucoma screening from
your eye doctor.

Picture of Glaucoma of the Eye
Diabetic
Retinopathy
·
·
The retina is
a group of specialized cells that convert light as it enters though the lens
into images. The eye nerve or optic
nerve transmits visual information to the brain.
Diabetic
retinopathy is one of the vascular (blood-vessel related)
complications related to diabetes. This diabetes eye problem is due to damage
of small vessels and is called a "microvascular complication." Kidney disease and
nerve damage due to diabetes are also microvascular complications. Large blood
vessel damage (also called macrovascular complications) includes complications
like heart disease and stroke.
The microvascular complications have, in numerous studies, been
shown to be related to high blood sugar levels. You can reduce your risk of
these eye problems in diabetes
complications by improving your blood sugar control.
Diabetic retinopathy is the leading cause of irreversible
blindness in industrialized nations. The duration of diabetes is the single
most important risk for developing retinopathy. So the longer you have
diabetes, the greater the risk of this very serious eye problem. If retinopathy
is not found early or is not treated, it can lead to blindness.
People with type 1 diabetes rarely develop retinopathy
before puberty. In adults with type 1
diabetes, it is also rare to see retinopathy before five years'
duration of diabetes. The risks of retinal damage increase with progressive
duration of diabetes. Intensive control of blood sugar levels will reduce your
risks of developing retinopathy. The DCCT, a large study of people with type 1
diabetes showed that people with diabetes who achieved tight control of their
blood sugars with either an insulin
pump or multiple daily injections of insulin were
50%-75% less likely to develop retinopathy, nephropathy (kidney disease), or
nerve damage (all microvascular complications).

Picture of Diabetic Retinopathy
of the Eye
People with type 2 diabetes usually have signs of eye
problems when diabetes is diagnosed. In this case, control of blood
sugar, blood
pressure, and blood cholesterol with diabetes have an important role
in slowing the progression of retinopathy and other eye problems.
Types of
Retinopathy in Diabetes:
- Background
retinopathy. Sometimes the blood vessel damage exists, but there is
no vision problem. This is called background retinopathy. It's important
to carefully manage your diabetes at this stage to prevent background
retinopathy from progressing to more serious eye disease.
- Maculopathy. In
maculopathy, the person has developed damage in a critical area called
the macula.
Because this occurs in an area that is critical to vision, this type of
eye problem can significantly reduce vision.
- Proliferative
retinopathy. New blood vessels start to grow in the back of the eye.
Because retinopathy is a microvascular complication of diabetes, a disease
of small vessels, this type of retinopathy develops because of an
increasing lack of oxygen to the eye from vascular disease. Vessels in the eye are
thinned and occluded and they start to remodel.
Here, it is important to address the risks factors that can
worsen the occluded vessels. Smoking cessation, high blood pressure control, cholesterol
management, and blood sugar control must take place in order to stop the
progression of new vessels from forming into the orbit of the eye. These are
fragile vessels that can bleed and eventually cause a clot to form in the
orbit, which scars and causes detachment of the retina. This
eventually leads to irreversible vision loss.
Treatment of diabetic retinopathy may involve laser procedures
or surgery. In a study of people with diabetes with early retinopathy, laser
therapy to burn the fragile vessel resulted in a 50% reduction of blindness.
To prevent retinopathy with diabetes, have your eye doctor
screen your eyes annually. Women with diabetes who later become pregnant should have a comprehensive eye exam
during the first
trimester and close follow-up with an eye doctor during the
rest of their pregnancy to avoid serious eye problems with
diabetes. (This recommendation does not apply to women who develop gestational diabetes, since they are not at risk for
retinopathy.)
Sources
© 2017 WebMD, LLC
মন্তব্যসমূহ
একটি মন্তব্য পোস্ট করুন