· Food Poisoning
20 Ways You Can Get Food Poisoning (
COURTECY;- WEBmd )

1/24
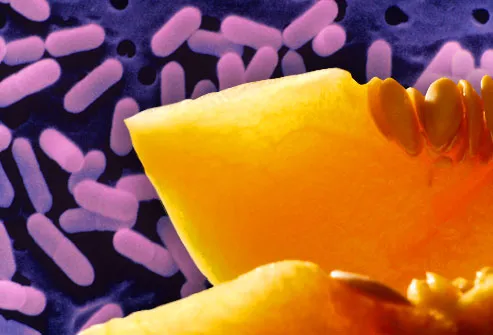
Listeria: Raw Fruits and Vegetables
Listeria bacteria can contaminate fresh
produce, like cantaloupes, as well as some processed foods, like cheeses.
Symptoms of infection include fever, muscle aches, upset stomach, or diarrhea
-- occurring 2 days to 2 months after exposure.
Safety: Scrub
raw produce and dry before cutting. Store in fridge below 40 F. Clean
everything in contact with a whole melon.

1/24
Listeria: Unpasteurized Dairy
Dairy products made with raw milk, including
yogurt and soft cheeses like Brie, feta, and Mexican queso, can harbor
listeria. Because listeria can live at colder temperatures, simply
refrigerating these foods won't kill the bacteria. People at highest risk of
getting sick include the elderly, pregnant women, and people with weakened
immune systems.
Safety: Check
the label. Make sure it's clearly marked "pasteurized."

1/24
Listeria: Deli Meats and Hot Dogs
Sometimes listeria finds its way into a food
processing factory, where it can live for years. Heat kills listeria, but
contamination may happen after cooking, but before packaging -- for
example, if a food is placed back on a counter that had raw meat on it.
Safety: Never
keep pre-cooked or ready-to-eat foods past their use-by date. Heat hot dogs and
lunch meats until steaming (165 F) before eating.

1/24
Salmonella: Poultry and Eggs
Salmonella bacteria can taint any food,
although there's a greater risk from animal products because of contact with
animal feces. In chickens, it can infect eggs before the shell forms, so even
clean, fresh eggs may harbor salmonella. Symptoms include stomach cramps,
fever, and diarrhea 12 to 72 hours after exposure. Illness usually lasts 4 to 7
days.
Safety: Never
eat raw or lightly cooked eggs. Cook poultry to 165 F. Keep raw poultry
separate from cooked poultry and other foods. Wash hands, cutting boards,
utensils, and countertops after handling.

1/24
Salmonella: Fresh Produce
Fresh produce is catching up with poultry as a
cause of salmonella infections. Outbreaks have been traced to tomatoes, hot
peppers, salad greens, and papayas. Sprouts, too, may harbor salmonella because
they’re grown in warm, humid conditions – and are often eaten raw or lightly
cooked. Infections can be severe or even fatal in people at higher risk,
including babies and the frail elderly.
Safety: Thoroughly
wash and dry produce, and store in the fridge at 40° F.

1/24
Salmonella: Processed Foods
Chips, crackers, soup, peanut butter, even
frozen meals may pose a slight risk for salmonella infection. One salmonella
outbreak was linked to peanut butter and packaged foods made with peanuts,
including granola bars and cookies. In cases like these, salmonella bacteria at
a processing plant can contaminate many products, which must then be recalled.
Safety: Never
use a product that has been recalled -- immediately return it to the store or
throw it away. Heating foods thoroughly to 165 F can kill salmonella bacteria.

1/24
Salmonella: Raw Meat
Raw meat, particularly ground meat, is at risk
for salmonella contamination. Ground turkey has been linked with several
salmonella outbreaks. You usually can't tell the food is contaminated because
it looks and smells normal.
Safety: Cook
beef, pork, and lamb to at least 145 F and poultry (including ground poultry)
to at least 165 F. Ground beef, pork, and lamb should be heated to 160 F. Avoid
cross-contamination by washing hands and all surfaces with warm soapy water
after contact with raw meat.

1/24
E. coli: Ground Beef
E. coli lives
in the intestines of cattle and can contaminate beef during the slaughtering
process. Ground beef is especially risky, because the bacteria can spread when
meat is ground up. Symptoms of E. coli infection include
severe abdominal cramps, watery diarrhea, and vomiting. The illness typically
develops several days after exposure and can be severe in vulnerable people. It
lasts about a week.
Safety: Cook
meat thoroughly (160 F, no pink in the center). Do not put a cooked burger back
on a plate that held raw meat. Wash utensils, including the meat thermometer,
with warm, soapy water.

1/24
E. coli: Raw Juice and Milk
Pasteurization uses heat to kill bacteria.
Since most juices you’ll find at the grocery store have been pasteurized, they
pose no risk. However, unpasteurized juices and ciders sold at farms, stands,
or in health food stores, can harbor E. coli. The
bacteria can also get into raw milk as a result of unclean milking equipment,
or manure-soiled or infected udders.
Safety: Buy
only products that have been pasteurized. If you're not sure, boil before
drinking.

1/24
E. coli: Fresh Produce
Fruits and vegetables can be tainted with E.
coli if the fertilizer or water used to grow them carries the bacteria. Leafy
greens are at highest risk. E. coli has been linked to fresh spinach. But
produce growers have put safety measures into place to minimize the risk.
Experts say the health benefits of eating fruits and veggies are far greater
than the risk of food poisoning.
Safety: Separate
and individually wash the leaves of leafy greens, and cook vegetables to kill
bacteria.

1/24
Botulism: Canned Foods
Botulism is a rare, potentially fatal illness
linked to improperly canned or preserved foods. Home-canned foods are especially
at risk, as well as honey, cured meats, and fermented, smoked, or salted fish.
Babies have the highest risk of getting sick. Symptoms include cramps,
vomiting, breathing problems, difficulty swallowing, double vision, and
weakness or paralysis. If you suspect botulism poisoning, call 911.
Safety: Never
give honey to children under 12 months. Throw away bulging cans, leaking jars,
or foul-smelling preserved foods -- or if liquid spurts out upon opening.
Sterilize home-canned foods by cooking at 250 F for 30 minutes.

1/24
C. Perfringens: Meat, Stew, and Gravy
Clostridium perfringens is a type of bacteria
that causes cramps and diarrhea lasting less than 24 hours. Stews, gravies, and
other foods that are prepared in large quantities and kept warm for a long time
before serving are a common source of C. perfringens infections.
Safety: Sauces,
gravies, and stews should be cooked thoroughly and then kept at a temperature
above 140 F or below 41 F. Serve food hot right after cooking. Promptly
refrigerate leftovers in shallow containers to allow for proper cooling.

1/24
Staph: Sandwiches, Salads, Pastries
Yes, you can get a staph infection from food
-- when an infected person prepares it. Foods at highest risk include
sandwiches, salads (including egg, tuna, chicken, potato, and macaroni),
cream-filled pastries, and puddings. Symptoms come on quickly, in as little as
30 minutes, and include vomiting, cramps, and diarrhea. The illness usually
runs its course in one to three days.
Safety: Wash
hands thoroughly before handling food. Do not handle food if you are sick or
have a nose or eye infection, an open wound, or infection on your hands or
wrists.

1/24
Hepatitis A: Improper Food Handling
Hepatitis A is a virus that attacks the liver
and can cause fever, fatigue, nausea, weight loss, and jaundice. Most
infections are mild. It can spread when an infected person doesn’t wash hands
properly, then touches food or items that are put in the mouth. Recent
outbreaks were traced back to workers in food processing plants or restaurants.
Safety: Get
vaccinated against hepatitis A. Check restaurant health ratings. Always wash
hands thoroughly before handling food.

1/24
Campylobacter: Undercooked Poultry
As little as one drop of raw chicken juice can
cause campylobacter illness -- a little-known illness that is the
second-leading cause of food poisoning in the U.S. Symptoms can include fever,
cramps, diarrhea, and vomiting. Most people recover in less than a week, but it
can lead to Guillain-Barre syndrome, a rare, serious illness. Guillain-Barre
develops a few weeks after diarrheal illness and can cause temporary paralysis.
Safety: Avoid
cross-contamination by washing hands, cutting surfaces, utensils, and
countertops in warm, soapy water after handling raw poultry. Cook poultry to at
least 165 F.

1/24
Norwalk Virus: Improper Food Handling
Noroviruses are the most common culprits in
what we think of as the "stomach flu." They cause vomiting and
diarrhea, and usually last 24 to 48 hours. Norwalk viruses contaminate food
when a food worker doesn’t wash his or her hands after using the restroom.
Foods like salad or raw shellfish pose a risk because they aren’t cooked before
eating.
Safety: Always
wash hands with hot, soapy water for 30 seconds after using the toilet or
changing diapers, and before handling food.

1/24
Vibrio Vulnificus: Raw Oysters
Vibrio vulnificus is
a bacteria that lives in warm seawater and can contaminate shellfish,
particularly oysters. V. vulnificus infection causes the same
gastrointestinal symptoms as many other foodborne illnesses, but in people with
weakened immune systems it can develop into a life-threatening blood infection.
Safety: Only
eat thoroughly cooked shellfish. Frying, baking, boiling, and steaming reduces
the risk of infection. Throw away any shellfish that doesn't open during
cooking.

1/24
Paralytic Shellfish Poisoning
Paralytic shellfish poison (PSP) is produced
by certain types of algae. When algae "blooms" -- called a red tide
-- it produces high levels of toxin and shellfish can be contaminated. Symptoms
of PSP include tingling lips and tongue, numbness, difficulty breathing, and
eventual paralysis. Death from PSP can happen as soon as 30 minutes after
extreme exposure. Luckily, PSP is extremely rare. Shellfish are regularly
tested for toxins before being sold to the public.

1/24
Scombrotoxin: Fresh Tuna
Scombrotoxin poisoning is an allergy-like
reaction to eating fish that has begun to spoil. Fish associated with
scombrotoxin include tuna, mackerel, amberjack, and mahi-mahi. In the early
stages of spoilage, bacteria produce histamines in the fish. This causes a
burning sensation in the mouth, itchy rash, dizziness, headache, and diarrhea.
Symptoms usually subside within four to six hours, and antihistamines can help.

1/24
Ciguatera Poisoning: Fish
This develops from eating reef fish like
grouper or snapper that have consumed some types of sea algae. Symptoms develop
within 6 hours of exposure and can include:
·
Burning or painful tingling in arms or legs
·
Headache
·
Nausea, vomiting
·
Diarrhea
·
Hallucinations
·
Temperature reversal (cold objects feel hot, hot objects feel
cold)
There is no cure for ciguatera poisoning, and although it usually goes away after days or weeks, neurological symptoms can sometimes last for years.

1/24
When to Call a Doctor
Most foodborne illnesses resolve on their own,
but you should call the doctor if you have:
·
A high fever
·
Bloody stools
·
Prolonged vomiting
·
Diarrhea lasting more than 3 days
·
Signs of dehydration (dry mouth, dizziness, reduced urination)

1/24
Tips for Safer Food Handling
·
Thoroughly wash hands before handling food.
·
Wash cutting surfaces, utensils, and countertops after contact
with raw meat.
·
Wash produce under running water and dry with paper towels.
·
Discard outer leaves of lettuce or cabbage.
·
Cook meat, poultry, and eggs to proper temperature.
·
Keep hot foods hot and cold foods cold.

1/24
Special Precautions
Certain groups are at increased risk of
contracting a foodborne illness or getting very sick from it. Pregnant women,
the elderly, young children, and people with compromised immune systems should
avoid eating undercooked meats and eggs, unpasteurized dairy products, uncooked
hot dogs and deli meats, and raw seafood.
This tool does not provide medical
advice.
মন্তব্যসমূহ
একটি মন্তব্য পোস্ট করুন